Nearly all people have low back pain at some point in their lives. In some industries, such as the trades and construction, chronic back pain is a significant problem at work, with 32% of workers over-indexing for just this condition.
Let’s learn more about back pain and what to do if you have a flare-up of low back pain:
Low back pain is defined as pain in the area between the lowest ribs and the buttock region. This area of the body is very mobile and allows us to bend forward, extend, bend side to side, and rotate.
Acute low back pain can make it difficult to move or find a comfortable sleeping position. It can also make you feel worried and anxious, which can make the pain worse. Chronic low back pain is defined as pain that lasts or recurs for at least three months. Unfortunately, chronic low back pain can lead to long-lasting sleep and mood problems.
For low back pain flare-ups, there are various nonpharmacological treatments available, such as:
• Heat or cold therapy
• Warm bath with magnesium salts
• Massage therapy and physical therapy
Additionally, there are positions that you can practice at home, such as the cobra pose or lying in the Z position (see image A) (image B).
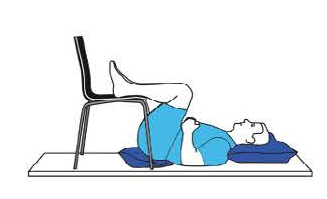
(A) ”Z” lie
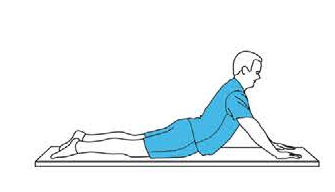
(B) Prone-lying passive extensions
Please speak with your healthcare provider if you have low back pain so they can rule out any serious problems. Since low back pain is often considered “non-specific,” it is advised to continue engaging in physical activity as much as possible. Exercise is the foundation of chronic back pain treatment. It’s one of the first treatments you should try under the guidance of your physician and spine physical therapist.
Other Pharmaceutical Treatments for Chronic Back Pain
Analgesics, anti-inflammatory drugs, muscle relaxants and other medications (ie. Opioids) can be used to help control chronic back pain. However, most come with unwanted side effects and are not intended for prolonged use. If you find yourself relying on opioids to get through the day, it may be time to seek a second opinion.
NEED TO SPEAK TO A HEALTHCARE PRACTITIONER ABOUT CHRONIC BACK PAIN?