People who are looking to use medical cannabis frequently ask: “what are the side effects, and is it addictive?” It is important to break down the answer depending on the patient’s unique circumstances and characteristics because there are many different factors at play in this complex question.
Is cannabis addictive?
Addiction, commonly known as substance use disorder, is possible with cannabis use. However, this is almost always only seen when large amounts of THC-dominant cannabis are taken recreationally rather than medicinally. In fact, a recent report from Health Canada on CBD found that it has a very low risk of abuse and is not habit-forming.1 This is consistent with the 2018 drug dependence WHO report.2
What are cannabis’ side effects?
The severity of any adverse effects associated with cannabis use—whether they are negative, unwanted, or unpleasant—must be considered. For instance, while cannabis can cause feelings of relaxation and well-being, some people may find these sensations unsettling.

The more severe chronic side effects of cannabis use, however, result from chronic, excessive use. These include problems with the lungs (caused by smoking), risk of worsening of mental health disorders in some individuals, and infrequently cannabinoid hyperemesis syndrome.
To avoid such side effects, healthcare practitioners advise:
· Use the lowest amount of THC possible for daytime symptom management
· Co-administer CBD
· Micro-dose THC using vaporizer, avoid smoking cannabis
· Take a 1–2 week cannabis holiday as needed
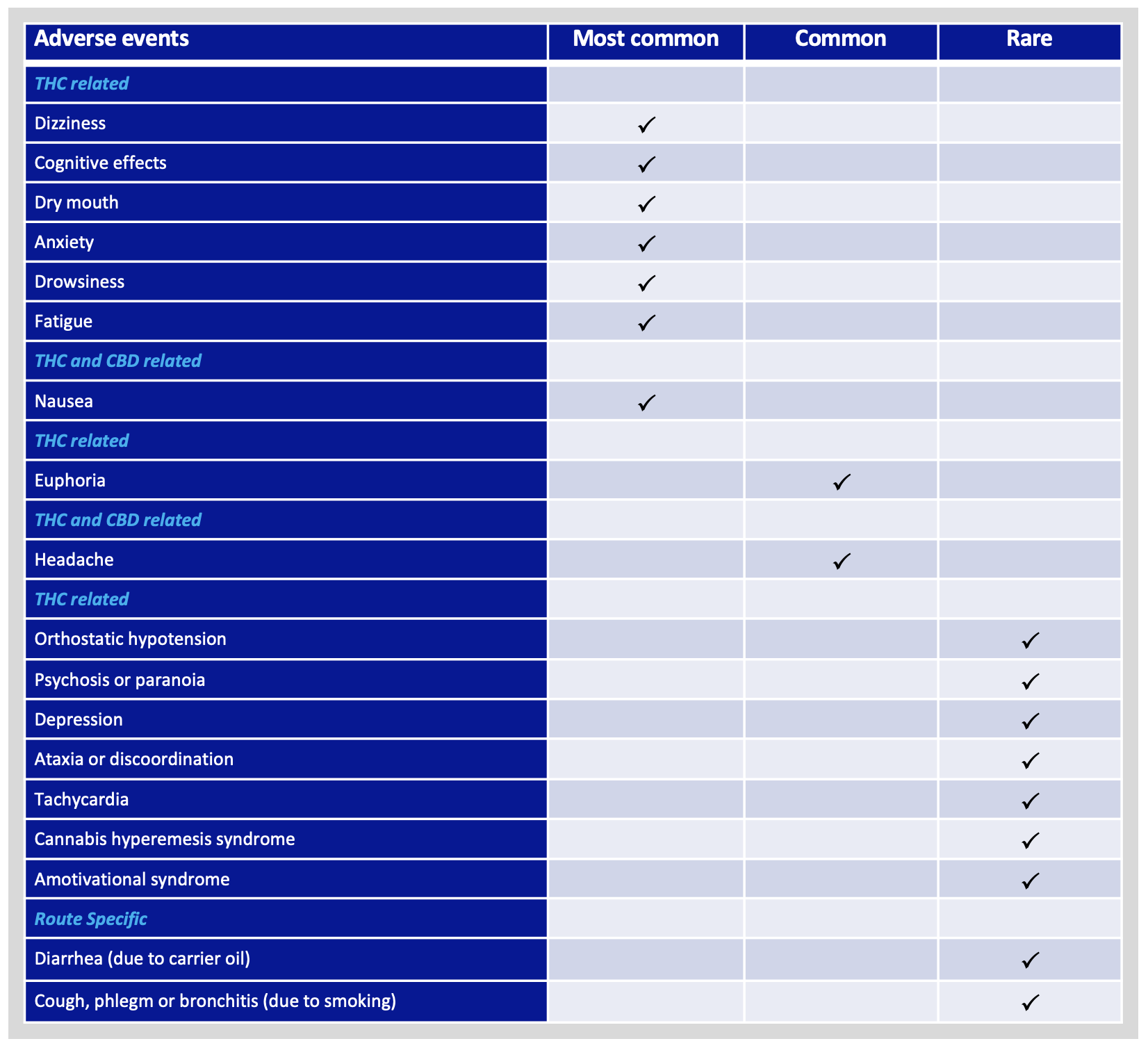
Common adverse events of CBD and THC
Cannabinoids like CBD and THC are well known for their analgesic, anti-anxiety, muscle relaxant, anti-inflammatory, and antiepileptic properties, among others. However, some individuals may experience unwanted and negative side effects, which typically depend on the dose and route of administration. See below for a summary of common adverse events.3
Health effects during pregnancy and breastfeeding

Just like many other substances and medications, a pregnant woman or new mother’s use of cannabis can affect her fetus or newborn child.4
Cannabinoids are carried through the mother’s blood to her fetus during pregnancy. They are also passed into the breast milk following birth. This can lead to health problems for the child including:
· Lower birth weight of the baby
· Decrease in memory function, ability to pay attention, and reasoning and problem-solving skills
· Increase risk for future substance use
Recommendations to avoid and limit unwanted health effects of cannabis 5
· Carefully follow your treatment plan and dosing instructions by your healthcare practitioner.
· Delaying cannabis use, at least until after adolescence, will lessen the likelihood or severity of adverse health outcomes.
· Use products with low THC content and high CBD.
· Synthetic cannabis products, such as K2 and Spice, should be avoided.
· Avoid smoking cannabis and choose safer inhalation methods including vaporizers.
· Do not drive or operate other machinery for at least 6 hours after using cannabis. Combining alcohol and cannabis increases impairment and should be avoided.
· Women who are pregnant or breastfeeding should not consume cannabis at all.
· People with a personal or family history of psychosis or substance use disorder have a higher risk for cannabis-related health problems and should consult with their healthcare practitioner about this.
What to do if you take too much THC
If you’ve mistakenly taken too much THC you might experience a sudden feeling of heightened sensations, panic, and uncomfortable “high”, which is also known as acute cannabis toxicity. There has been an increase in first-time cannabis users across Canada who may not be aware of the many effects of cannabis, their physiological tolerance, and the delayed onset of symptoms seen with some routes of ingestion6.
Although you cannot die from a cannabis overdose, the following supportive care practices should be kept in mind:
· Completely avoid any dangerous behaviour, such as driving, operating machinery, being around children, or consuming other substances like alcohol.
· Call a trusted family member or friend who will be there for you and offer comfort.
· Visit your local emergency department if you have severe intoxication symptoms including chest pain, mental health crisis, or extreme nausea and vomiting.
· For cannabis hyperemesis syndrome (i.e., cannabis-induced nausea and vomiting), limited evidence suggests that applying topical Capsaicin cream to the abdomen may help alleviate symptoms within 30 to 45 minutes.7
· The effects of cannabis typically last longer at higher THC concentrations.
· Effects from inhaled cannabis usually last 2-4 hours, and ingested cannabis usually lasts 8-12 hours.
· Keep calm. Most symptoms will dissipate within minutes to hours.
· Keep hydrated with water and eat healthy snacks like fruits, nuts, or cheese.
· Although there is no medical literature to support it, some cannabis connoisseurs recommend chewing a black peppercorn.
· Find a quiet place without a lot of stimuli where you can keep calm, breathe deeply, and rest.
· Take a shower to relax the mind and body. Some research indicates that cold showers can help you feel more alert and grounded.
· Distract yourself by engaging in calming activities like colouring, talking to trustworthy friends, or listening to your favourite music.
Reporting adverse events
Please let us know if you have experienced an adverse event. As a licensed producer under the Cannabis Act, we have procedures in place to appropriately report adverse reactions to Health Canada.

Call or email Starseed Client Care Team at 1-844-756-7333 or info@starseed.com