Previous Article
Talking about Cannabis with your Friends and Family Members
You'll probably be spending more time with your family, friends, and loved ones now that the holidays are approaching. The reality of these lifelong relationships is that occasionally our personal beliefs and opinions may start to diverge from those of some of the people we value most. Cannabis tends to be one of these hot topics, so we have put together some talking points on how to bring up cannabis with people in your life who might not share your knowledge and beliefs regarding cannabis-based medicine.
Why is it hard to talk about cannabis?
Cannabis has a turbulent history, and in the 1930s, American politicians stigmatized cannabis for a variety of reasons, some of which were just racist. Politicians told Congress that "marijuana is an addictive drug which produced in its user's insanity, criminality, and death" while having no medical or scientific evidence to support their claims.
Cannabis was misunderstood and vilified for a very long time. It was sometimes referred to be a "gateway drug" to stronger drugs. Cannabis is currently, however, is demonstrated by researchers to be an "exit drug" and a potentially effective tool in the fight against the opioid crisis.
At the very least, we can replace a medicine that has the potential to kill people (opioids) with one that does not (cannabis). According to data from the United States, medical cannabis laws have lowered opioid prescribing in every state where they have been implemented1.
Cannabis is now legal in Canada
In Canada, laws and regulations have advanced significantly. Canada is the first major industrialized country to legalize access to cannabis for both medical and non-medical uses, and it is widely available for purchase.
How do you access legal medical cannabis?
A medical cannabis clinic like North Stars Wellness or HelloMD provides access to a medical professional who assesses and then authorizes medical cannabis for purchase from a licensed producer (like Starseed Medicinal) and provides medical cannabis education and tailored treatment plans. With medical authorization, a patient can deduct the cost of medical cannabis from their taxes and, if their insurance policy covers it, use its benefits for medical cannabis.
The provincial government regulates adult-use (i.e., recreational) cannabis that is sold in retail cannabis stores from licensed producers. However, there are many restrictions on what sales representatives (i.e., budtenders) in cannabis retail stores are allowed to say. For instance, they are not allowed to make any health claims or imply a health or cosmetic benefit. People should speak with a healthcare professional about the potential medical benefits of cannabis for this reason.
The Cannabis Act, which is enforced by Health Canada and includes stringent controls and quality assurance testing, governs all licensed producers of cannabis for both medical and non-medical use.
How to talk about medical cannabis
1. Choose a comfortable and safe setting and approach
Talking to people one-on-one is frequently preferable. When you plan this conversation, keep in mind to do it in a relaxed environment where you and your loved one can effectively discuss your cannabis therapy and their concerns.
Do not minimize their concerns and encourage them to openly ask questions. Take your approach to science, a subject where they have less room to disagree, rather than becoming frustrated or defensive.
2. Highlight scientific research and the benefits to your quality of life
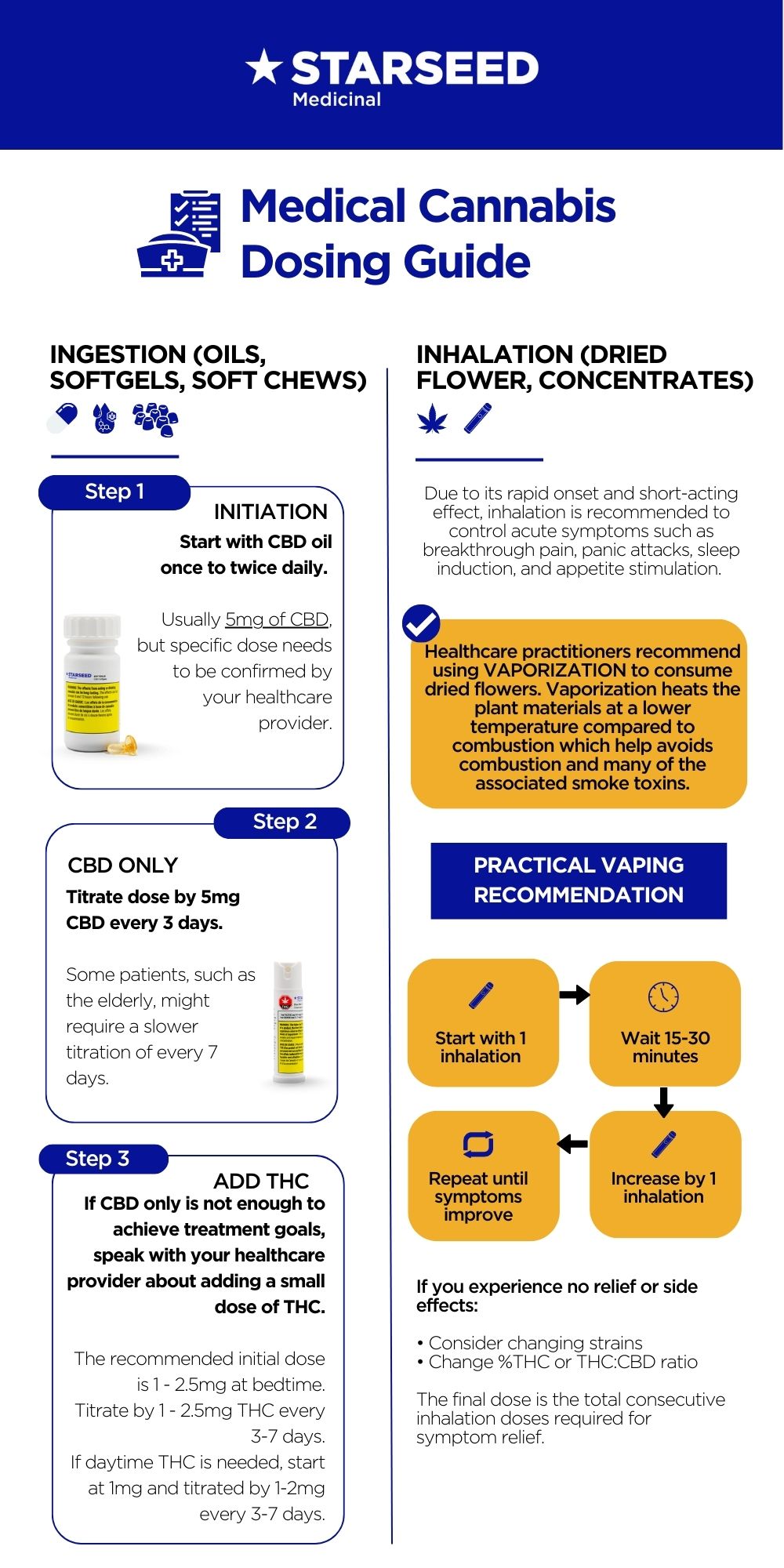
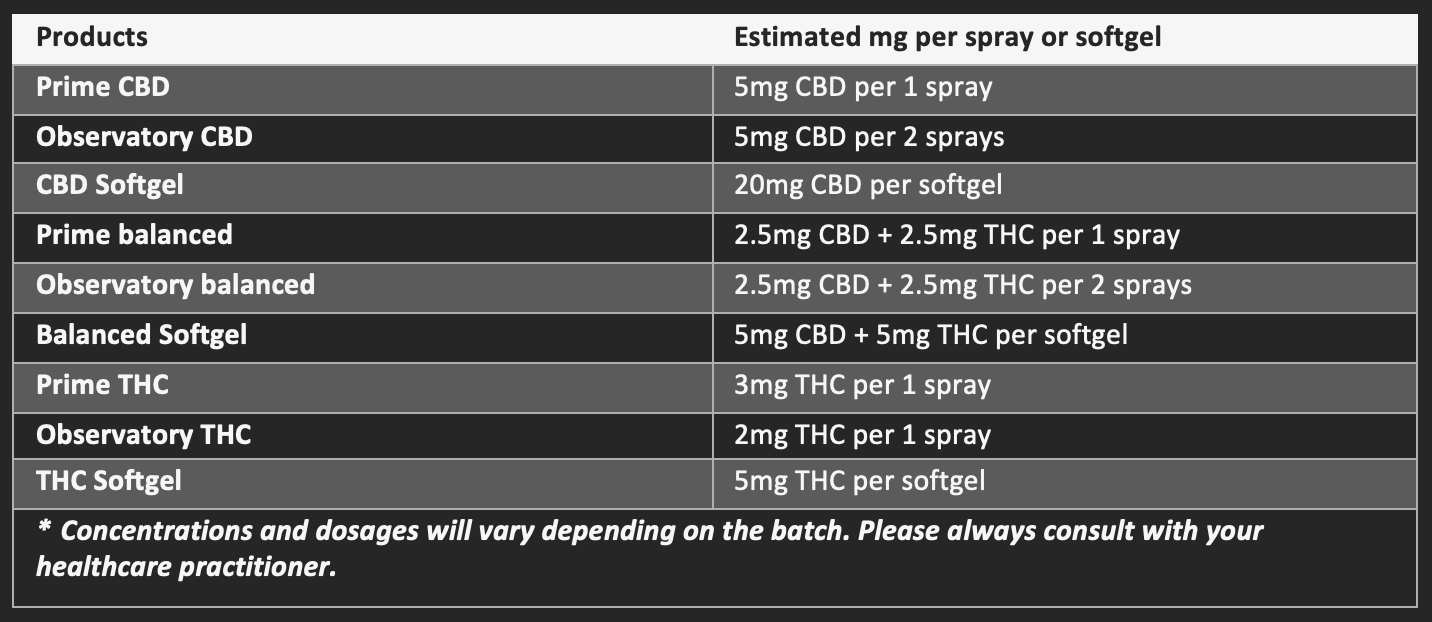
Being prepared with research is one of the best things you can do when discussing your experience as a medical cannabis patient. You might start by giving them a general overview of the plant, comparing THC with CBD, and discussing the many formulations (oils and topicals), or you could just get right to tell them how it has specifically helped you.
If you’re diagnosed with a condition like chronic pain, anxiety, sleep disturbances, or arthritis, for example, use scientific studies to back up your reason for turning to medical cannabis.
3. Dispel the myths that cannabis is all about getting you high and smoking joints
Fact: Cannabis contains more than 150 active compounds, 2 of which are CBD and THC – the prime compounds that are used in medical cannabis. THC is responsible for the psychoactive intoxicating effects, a.k.a the feeling of being “high”. CBD is non-intoxicating and doesn’t produce any “mind-altering” effects. Starseed patients can opt to use CBD-dominant products with little or no THC to avoid the intoxicating effects.
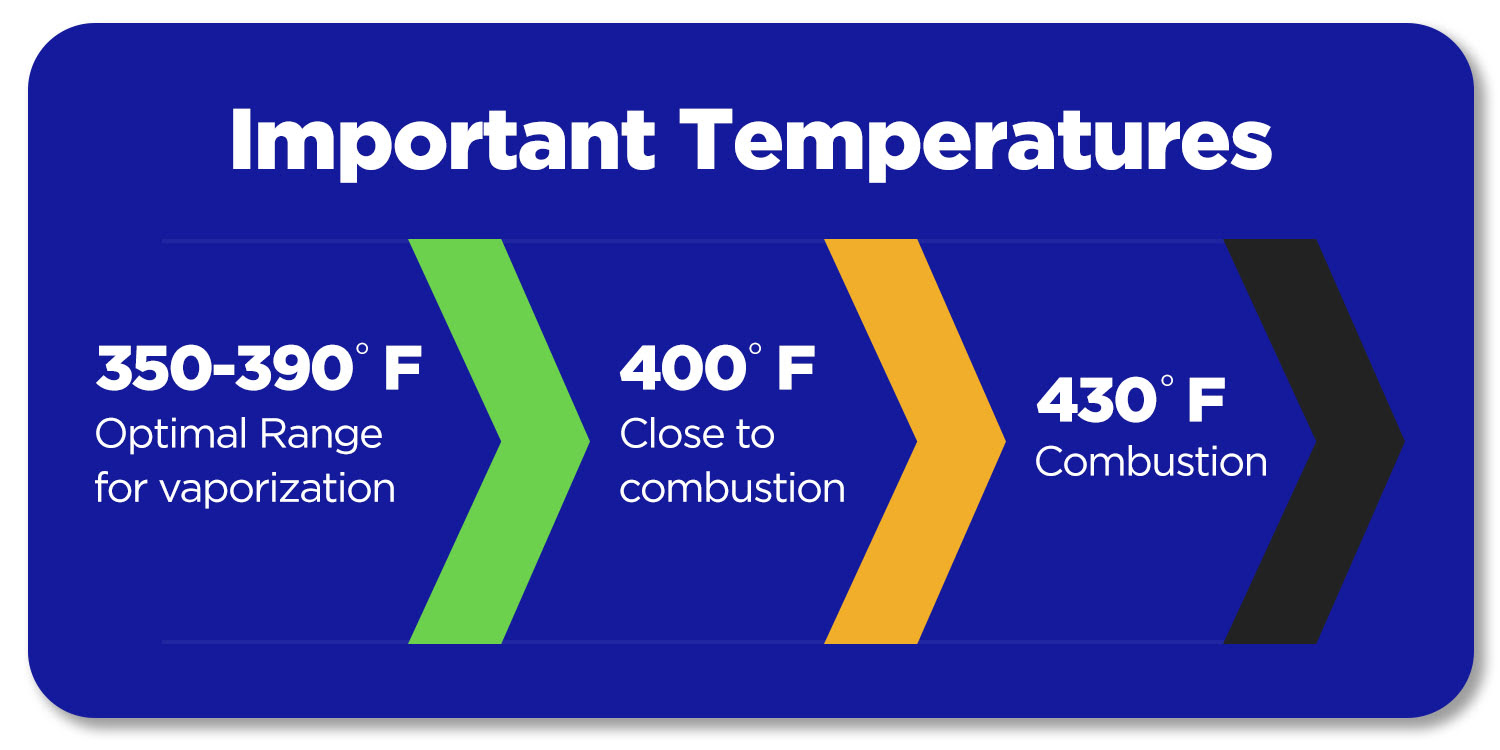
Fact: Medical cannabis can be consumed in multiple ways besides smoking, such as ingestion or skin application. Although inhaling cannabis has a rapid onset and shorter duration of action, smoking (or burning) cannabis is not advised due to the toxic by-products of smoke, such as ammonia, nitrous oxide, and compounds known as PAHs, which are all potentially carcinogenic. Furthermore, not only can burnt plant products and paper irritate your lungs and cause you to cough, but much of the medicine burns up too quickly.
4. Talk about your treatment plan
Your medical cannabis treatment plan acts like a prescription and offers the specific dosage instructions and product recommendations made by your healthcare practitioner, enabling you to follow a safe and responsible medical cannabis regimen with confidence.
5. Talking to kids about cannabis
It might be difficult to know how to communicate with kids about cannabis. You should use Drug-Free Kids Canada as a great resource for having these difficult conversations.
If you have any other questions about cannabis, registration or booking an appointment with a Healthcare Practitioner, please contact our Client Care Team at 1-844-756-7333 or info@starseed.com.
[1] Bradford, A. C., Bradford, W. D. Medical Marijuana Laws Reduce Prescription Medication Use In Medicare Part D. Health Aff (Millwood) 35, 1230–1236 (2016)
Bradford, A. C., Bradford, W. D., Abraham, A. & Adams, G. B. Association Between US State Medical Cannabis Laws and Opioid Prescribing in the Medicare Part D Population. JAMA Intern Med (2018)
Wen, H. & Hockenberry, J. M. Association of Medical and Adult-Use Marijuana Laws With Opioid Prescribing for Medicaid Enrollees. JAMA Intern Med (2018)
Next Article
Cannabis and Dementia
According to the Alzheimers society in Canada, by the 2040s it is expected that 20,000+ Canadians will be diagnosed with dementia every month1. In Ontario, 64% of long-term care residents have a diagnosis of dementia2. Neuropsychiatric symptoms (behavioural and psychological symptoms in dementia) are on the rise and can be challenging to treat as our population ages and people with dementia live longer.
The therapeutic potential of cannabinoids has been studied by researchers and clinicians over the past decade. They have investigated a range of topics, including whether cannabinoids can improve the neuropsychiatric symptoms of dementia such as agitation, mood changes, apathy, psychosis, wandering, and aggression.
An exciting, new placebo-controlled, randomized clinical trial has just been published to evaluate the safety and efficacy of CBD-dominant medical cannabis oil for the reduction of behavioural disturbances amongst patients with dementia. The formulation of the CBD oil is 30% (or 295mg/mL) CBD and 1% THC (or 12.5mg/mL). They found a statistically significant reduction in agitation over placebo with non-serious side-effects3.
These research findings are not surprising, given the therapeutic potential of CBD for anxiety and psychosis 4,5. According to studies, CBD may have antipsychotic and anxiolytic benefits, but more importantly, it can protect patients against the negative side effects of some of the available drug therapies.
We know that agitation is a common change in behaviour in people with dementia. Many also agree that non-drug treatments should be used before turning to drugs for acute agitation that doesn't improve with other measures. Existing medications can be used to treat behavioural changes like agitation, but many of them have harmful side effects. For example, antipsychotics often only provide a temporary relief and come with serious risks like the potential of falls, strokes, or even death 6,7.
More than 1 in 5 residents of long-term care centers receive antipsychotics off-label and without a diagnosis, according to recent research8. The Canadian Institute for Health Information (CIHI) reports that since the pandemic started, the off-label use of antipsychotics has increased9.
Cannabinoids, on the other hand, interact with the body different, which means they could be safer and more effective overall for someone experiencing agitation. Some of their actions are even said to help prevent the loss of brain cells, but human clinical trials have not yet shown evidence to support this notion10.
For those who have dementia, weight loss, pain, and sleep issues are major issues that are frequently accompanied by agitation and aggression. Cannabinoids have also been associated with improvements in appetite and pain11.
A diagnosis of dementia may be upsetting for you and your friends and family. If you are a family member or friend, there are things you can do right now to make life a little easier. Find out more at Alzheimer’s Society in Canada.
Potential harms of antipsychotics:
• Side effects including sedation, falls, postural hypotension, confusion, stiffness/rigidity, diabetes, constipation, and weight gain
• Increased risk of stroke
• Increased risk of death
Health Canada noted a 1.6-fold increase in mortality (mostly related to heart failure, sudden death pneumonia). Some data suggests that there will be 1 extra stroke or death for every ~100 people treated with antipsychotics13.
[1] Alzheimer Society of Canada. (2022). Navigating the path forward for dementia in Canada. The Landmark Study Path. Retrieve from https://alzheimer.ca/sites/default/files/documents/Landmark-Study-Report-1-Path_Alzheimer-Society-Canada.pdf
[2] Ontario Long Term Care Association. (2019). This is long-term care 2019. Retrieved from https://www.oltca.com/OLTCA/Documents/Reports/TILTC2019web.pdf
[3] Hermush, V., Ore, L., Stern, N., Misrahi, N., Fried, M., et al. (2022). Effects of rich cannabidiol oil on behavioural disturbances in patients with dementia: a placebo controlled randomized clinical trial. Frontiers in Medicine. Retrieved from https://www.frontiersin.org/articles/10.3389/fmed.2022.951889/full#h15
[4] Zuardi, A.W., Rodrigues, N.P., Silva, A.L., Bernardo, S.A., Hallak, J.E.C., et al. (2017). Inverted u-shaped dose-response curve of the anxiolytic effect of cannabidiol during public speaking in real life. Front Pharmacol, 8, 259.
[5] Schubart, C.D., Sommer, I.E., can Gastel, A., Goetgebuer, R.L., Kahn, R.S., Boks, M.P. (2011). Cannabis with high cannabidiol content is associated with fewer psychotic experiences. Schizophr Re, 130 (1-3), 216-221.
[6] Fraser, L., MMath,K.L., & Naylor, K.L. (2015). Falls and fractures with atypical antipsychotic medication use: A population-based cohort study. JAMA Internal Medicine, 175(3), 450-452.
[7] Wang, P.S., Schneeweiss, S., Avorn, J., Fischer, M.A., Mogun, H., Solomon, D.H., & Brookhart, A. (2005). Risk of death in elderly users of convention vs. atypical antipsychotic medications. The New England Journal of Medicine, 353 (22), 2335-2341.
[8] https://www.cbc.ca/news/canada/antipsychotic-medication-seniors-long-term-care-1.6581304
[9] Canadian Institute for Health Information. Potentially Inappropriate Use of Antipsychotics in Long-Term Care. Accessed November 22, 2022.
[10] Shelef, A., Barak, Y., Berger, U., Paleacu, D., Tadger, S., Plopsky, I., & Baruch, Y. (2016). Safety and efficacy of medical cannabis oil for behavioural and psychological symptoms of dementia: An open- label, add-on, pilot study. J Alzheimers Dis, 51, 15-9. 5
[11] Volicer, L., Stelly, M., McLaughlin, J., Volicier, B.J. (1997). Effects of dronabinol on anorexia and disturbed behavior in patients with Alzheimer’s disease. Int J Geriatri Psychiatry, 12(9), 913-919.
[12] Centre for Effective Practice. (April 2016). Use of Antipsychotics in Behavioural and Psychological Symptoms of Dementia (BPSD) Discussion Guide: Long-Term Care (LTC 2nd Edition)
[13] Health Canada. Atypical antipsychotic drugs and dementia – advisories, warnings and recalls for health professionals [Internet]. 2005. Available from: http://www.healthycanadians.gc.ca/recall-alert-rappel-avis/ hc-sc/2005/14307a-eng.php.