People are increasingly turning to cannabis as an alternative to other conventional methods of treating their condition’s symptoms. Several myths and misconceptions continue despite research advancements and mounting data that supports the use of medicinal cannabis.
Due to the extensive misinformation regarding medical cannabis that has been spread over the years, several myths have developed. To decide if medical cannabis is right for you, you must first gather correct information and separate fact from myth. The most prevalent myths regarding medical cannabis are listed here. Let’s separate the facts from fiction!
1. All medical cannabis products get you “high”
Fact: Cannabis contains more than 150 active compounds, 2 of which are CBD and THC – the prime compounds that are used in medical cannabis. THC is responsible for the psychoactive intoxicating effects, a.k.a the feeling of being “high”. CBD is non-intoxicating and doesn’t produce any “mind-altering” effects.1 Starseed patients can opt to use CBD-dominant products with little or no THC to avoid the intoxicating effects.
2. Smoking medical cannabis is the most effective method of pain relief
Fact: This is false. Medical cannabis can be consumed in multiple ways besides smoking, such as ingestion or skin application. Although inhaling cannabis has a rapid onset and shorter duration of action, smoking (or burning) cannabis is not advised due to the toxic by-products of smoke, such as ammonia, nitrous oxide, and compounds known as PAHs, which are all potentially carcinogenic. Furthermore, not only can burnt plant products and paper irritate your lungs and cause you to cough, but also, much of the medicine burns up too quickly.
Visit our Product Guide to view the most common methods of consumption and their effects.
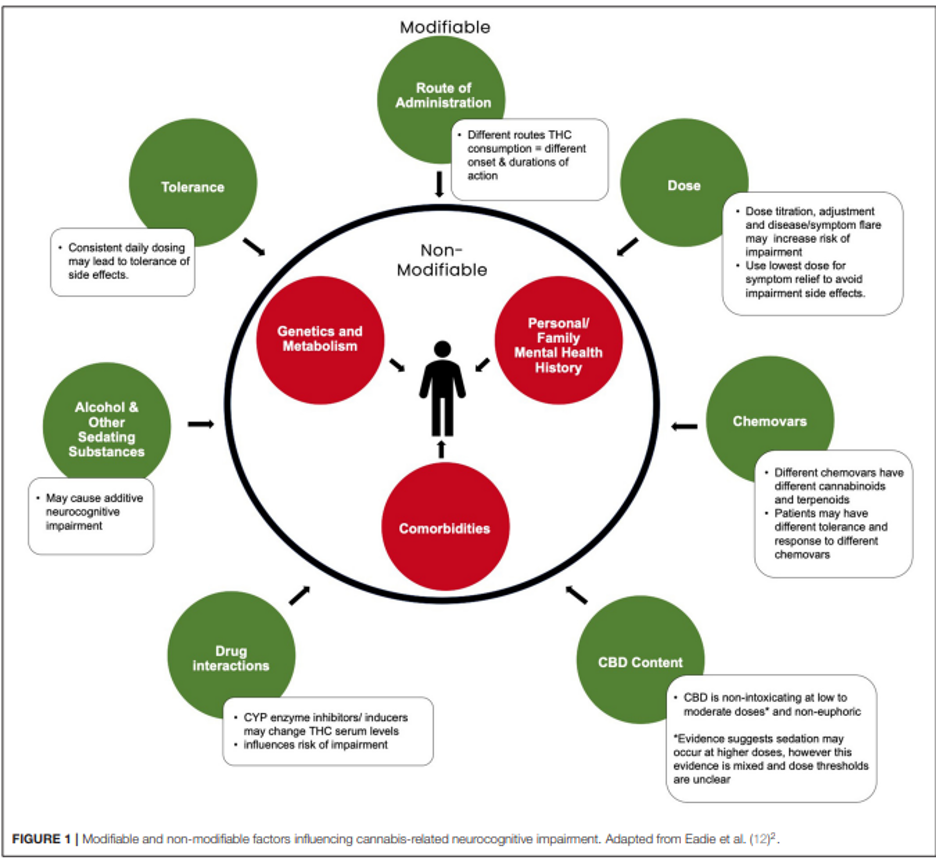
3. Using the same chemovar (or strain) or cannabis product will give everyone the same result
Fact: Each person will be affected differently depending on the amount of THC and CBD, the frequency, and the duration of consumption. Different chemovars will contain varying amounts of terpenes and cannabinoids. The effects of chemovars and cannabis products vary greatly depending on the patient and are influenced by a variety of both controllable and uncontrollable factors, as illustrated in the figure below.2 Therefore, in order for medical cannabis patients to benefit the most from their treatment, it’s crucial that they have an assessment with a healthcare professional regarding expectations, dose instructions, and follow-up sessions.
4. Higher THC/CBD potency means better medical cannabis quality and better effects
Fact: Cannabis with a higher THC and/or CBD content doesn’t necessarily work better. Only when the cannabinoid content and dosage of medical cannabis are customised for you and your condition will it be most effective.
The benefits of medical cannabis go beyond just higher cannabinoids potency. You must take into account the dosage and your symptoms or medical condition. For instance, Star-1 or Star-3 cannabinoid profile products may not be as successful if your treatment plan asks for a Balanced product with a 1:1 mix of CBD and THC.
5. THC is better for pain relief (or vice versa)
Fact: There’s no definitive answer to the debate between THC and CBD for pain relief. The THC to CBD ratio in your medical cannabis should ideally match the one recommended by a healthcare professional for your condition. High-THC products may not be effective for all people with pain, and vice versa. Below is a general overview of THC and CBD.
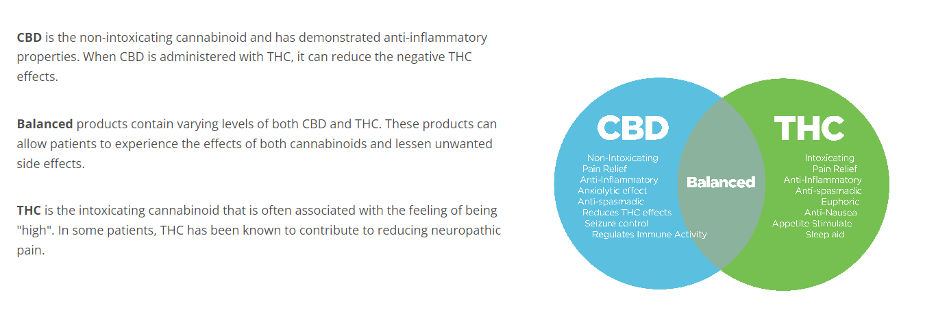

As always, we recommend patients start low and go slow with medical cannabis and stick with their treatment plan guided by a Healthcare practitioner for the best results. Scheduling regular checkups is also a great way to stay on top of your treatment.