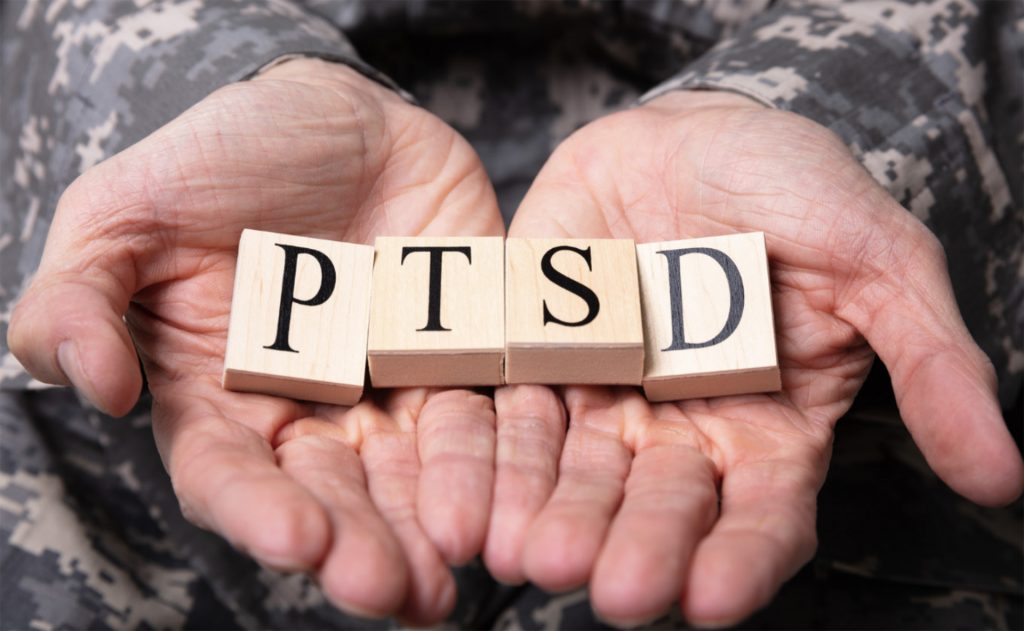
Post-traumatic stress disorder (PTSD) is a debilitating condition affecting millions worldwide. It is a mental health disorder that can develop after experiencing or witnessing a traumatic event. The symptoms of PTSD can be severe and include flashbacks, nightmares, hypervigilance, and anxiety. The coexistence of PTSD with other mental health conditions such as anxiety disorders, depression, insomnia, and substance use disorders makes treatment even more challenging.
Psychotherapy and medications such as antidepressants, antianxiety medications, and antipsychotics are the mainstay treatments for PTSD. These treatments might not always work and could have significant side effects, especially if more than one medication is taken at a time. People with PTSD are often desperate for a treatment that works well and has few side effects. Some people with PTSD may have discovered that cannabis reduces nightmares, promotes sleep, and calms anxiety and irritability.
The endocannabinoid system (ECS) is a biological system that plays a crucial role in regulating various physiological processes, including mood, stress response, and memory. The ECS is activated by cannabinoids, which can help to modulate the stress response and reduce anxiety.
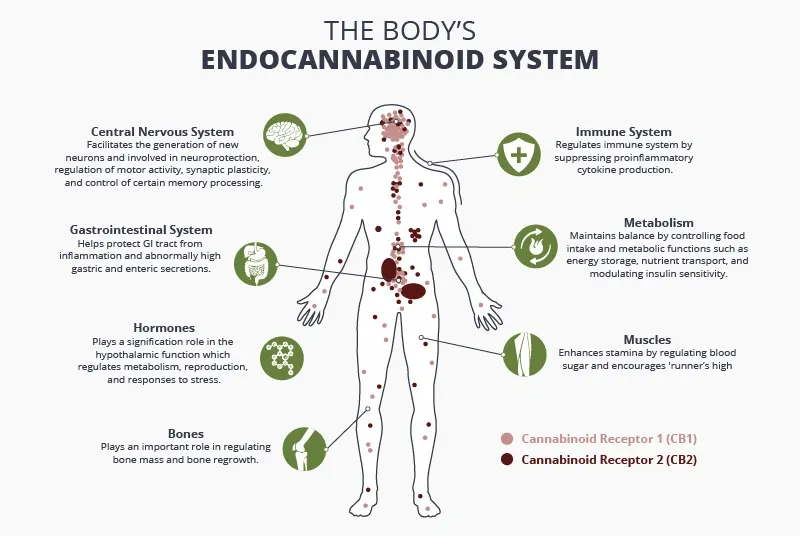
As the number of veterans suffering from PTSD has greatly increased over the past few decades, understanding how cannabis may benefit individuals with this condition is an important area of research. The amygdala in the brain, which controls anxiety, fear memories, and emotional responses to stress, has been found to have high levels of cannabinoid receptor expression. A well-functioning ECS must exist in order to have an adaptive response to fear and to the associated traumatic memories.
Although published research on the use of cannabis for PTSD is limited, there are some studies to suggest that medical cannabis may be helpful in managing PTSD symptoms.
A randomized, double-blind, placebo crossover study from Canada found that nabilone, a synthetic THC, dramatically reduced the severity and frequency of nightmares and improved general well-being in a small sample of military veterans with treatment-resistant PTSD.In a study published in the Journal of Psychoactive Drugs, 75% of participants with PTSD reported a decrease in symptoms after using medical cannabis.
According to preclinical studies, CBD may inhibit the formation, expression, and reconsolidation of fear memories. The effects of CBD on PTSD patients have only been studied in a small number of human trials, which lack high-quality evidence and call for more research. However, CBD has also been shown to have anxiolytic effects, which could help to alleviate the anxiety and hypervigilance associated with PTSD.

Even though cannabis is becoming more recognized as a potential treatment for PTSD, the concept of receptor downregulation with THC use is critical for patients to understand. Keep in mind that prolonged, heavy use of cannabis with a high THC contentwill reduce the number of cannabinoid receptors, which will eventually cause tolerance and a loss of effectiveness. Cannabis with a high THC content must be used with caution by patients with PTSD to avoid tolerance and maximize effectiveness.
Pro-tip for THC:
• Use lowest amount of THC possible for symptom management
• Co-administer CBD
• Micro-dose THC using vaporizer, avoid smoking cannabis
• Take 1-2-week cannabis holiday as needed
It’s important to note that while medical cannabis may be a potential treatment option for PTSD, it is not a cure for the condition. PTSD is a complex disorder that requires a comprehensive treatment approach, including therapy, medication, and lifestyle changes.
Medical cannabis should be used in conjunction with other treatments under the guidance of a healthcare professional. Need help connecting with a Healthcare professional for Medical cannabis?